What Does “Borderline High Sugars” Really Mean? An URGENT Wake-up Call !!!
What Does “Borderline High Sugars” Really Mean? An URGENT Wake-up Call !!!
By John Sciales, M.D.
Founder & Director, CardioCore Metabolic Wellness Center
“Getting to the Core… the Path to Wellness — where being Healthy is Not an Accident.”
Abstract
🚨 There is no such thing as “borderline.”
You can’t be “a little pregnant,” and you can’t have “a little diabetes.” By the time your blood sugar is labeled “borderline,” the underlying process has been going on for years. Gone are the days when one is told "watch your diet, cut back on the sweets and follow up in 6 months." This advice is archaic but sadly for many physicians, it remains the default setting like pushing a button on a computer.
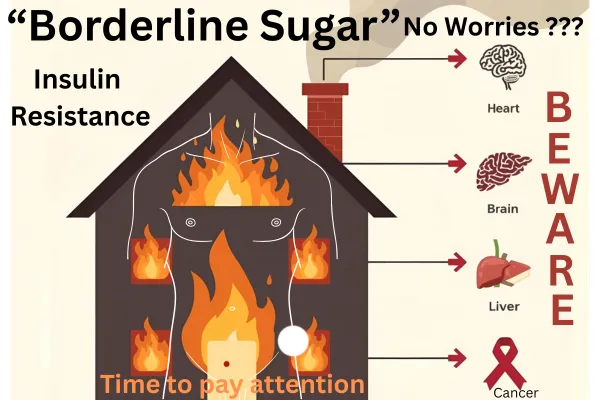
'Borderline sugar' isn’t a small warning sign ... it’s an eye-opening event. It means your body has been living with insulin resistance, silently pushing insulin higher and higher just to keep sugars in range over the last 10-20 years. During that time, plaque may already be forming in your arteries, your liver may be storing fat, your brain may be under metabolic stress, and your risk for cancer may be climbing.
That’s why “borderline” isn’t a stage to watch and wait. It’s a turning point that calls for action. The real problem isn’t sugar itself — it’s insulin resistance; the core driver of a multifaceted and insidious process that has long term consequences. Sugar is just a late manifestation, very late. And unless it’s recognized and addressed early, the next step is not just diabetes, but heart disease, dementia, liver failure, and more. Unfortunately these issues may not be emerging consequences, but rather already entrenched simmering beneath the water, waiting to resurface.
👉 Borderline sugar is NOT a soft warning — it’s a red alarm telling you the clock has been ticking for a long time.
📖 The following article explains why “borderline” should never be brushed aside and why shifting the focus from sugar to insulin is the only way to prevent disease before it’s too late.
Introduction: Borderline But Not Benign
Imagine this: You go to your doctor for a routine check-up. Your blood work comes back, and the doctor says, “Your sugars are a little borderline — just watch your diet and maybe lose some weight. No need for medication yet.” Or maybe the doctor doesn’t even mention it at all, and you only notice the elevated value when you look over your labs yourself.
It sounds harmless, even reassuring. But in reality, that single word — “borderline” — hides the truth: your body has already been battling diabetes for a decade or more (1–4).
Think of it this way: glucose is the smoke. Insulin resistance is the fire.
Traditional medicine’s glucose-centric model is like watching a house burn and waiting until the flames are visible on the roof before calling the fire department (3,4). By the time your blood sugar is “borderline,” the fire has been raging quietly for years.
Another way to picture it is the football analogy. In type 2 diabetes, your body’s cells slowly stop listening to insulin. It’s like a husband watching football, not hearing his wife. What does she do? She talks louder and louder until he finally listens. That’s what your pancreas does — it shouts louder by producing more and more insulin (4).
Doctors call this stage prediabetes. Too often it’s dismissed with: “You don’t need medication yet.” But the truth is, this stage means your pancreas is already approaching exhaustion — and elevated sugar is one of the last manifestations of insulin resistance, not the first (1,5).
Key Takeaway: Borderline sugars don’t mean “safe” or “early.” They mean the disease has been burning silently for years — and your pancreas is nearly spent.
The Timeline of Beta-Cell Burnout
Your pancreas contains beta cells, the factory workers responsible for making insulin — the hormone that moves sugar from your bloodstream into your cells for energy (4).
When your body becomes resistant to insulin, those beta cells work overtime to keep blood sugar normal. But they can only shout for so long before burning out (3,4).
Here’s how the journey unfolds:
Early insulin resistance (10–15 years before “borderline” sugars):(4).
Muscle, liver, and fat cells stop responding to insulin.
The pancreas compensates by making extra insulin (hyperinsulinemia).
Blood sugar looks normal — but the fire has already started.
Pancreatic Compensation Phase (5–10 years in)
Fasting insulin levels double or triple.
Blood pressure starts rising.
Cholesterol shifts (low HDL, high triglycerides).
Inflammation smolders.
Silent atherosclerosis begins.
Beta-cell Fatigue (10+ Years in )
Beta cells lose strength.
After ~85% burnout, hemoglobin A1c finally creeps into the “borderline” zone (5.7–6.4%).
At ~90% burnout, sugars rise into the diabetic range.
So when a doctor says, “You’re just borderline,” what they’re really saying is: “Your pancreas is almost exhausted.”
Beta cells lose strength.
After ~85% burnout, hemoglobin A1c finally creeps into the “borderline” zone (5.7–6.4%).
At ~90% burnout, sugars rise into the diabetic range.
The tragedy is that many patients — and even many clinicians — think borderline high sugar is the beginning of diabetes. In truth, it’s the end of a long, silent journey where insulin resistance has already been damaging your heart, brain, liver, and cancer risk for more than a decade
Key Takeaway: Prediabetes is not an early phase. It is a late phase — the final stage of insulin resistance after 10–15 years of silent damage, with 85–90% beta-cell burnout already present.
Insulin Resistance: The Silent Fire
Insulin resistance doesn’t just affect sugar. It quietly damages almost every organ in the body years before blood sugar ever rises.
Heart & Blood Vessels
Insulin resistance fuels inflammation and reduces nitric oxide, driving high blood pressure, arterial stiffness, and plaque buildup (3,4,7,8). Since 2013, major societies (AHA, ADA, ESC) have agreed: diabetes is a cardiovascular disease equivalent — having it carries the same heart attack risk as existing heart disease (6,18).
Cancer
Insulin is also a growth signal. Cancer cells exploit this by having 10–50x more insulin receptors than normal cells, making high insulin a powerful tumor fertilizer (11,12).
The data:
Breast cancer: 20–40% higher risk with BMI >30
with severe obesity with BMI >40, breast cancer risk ~4.6x higher (13,14).
Uterine cancer (endometrial): Skyrockets with BMI
Endometrial cancer risk: BMI 30–35 → 152% higher than normal
BMI 35–40 → 345% higher than normal
BMI >40 → 614% higher than normal (13,14).
Even “borderline sugars” combined with obesity and insulin resistance place women at dramatically higher cancer risk.
Dementia & Brain Health
After genetics, the strongest risk factor for dementia is insulin level, not cholesterol or smoking (9). High insulin damages brain energy use, contributing to Alzheimer’s (often called “type 3 diabetes”) (10).
Insulin resistance also plays a role in Parkinson’s disease, linking metabolism to motor and cognitive decline (9,10).
Fatty Liver
Insulin resistance also traps fat in the liver, leading to MASH (Metabolic dysfunction-Associated Steatohepatitis). This condition is no longer considered harmless — in fact, MASH is now the leading cause of cirrhosis and liver failure requiring liver transplant, surpassing both alcohol-related disease and viral hepatitis. (15–17). A fatty liver is not just a liver problem — it’s a sign that the entire body is metabolically sick.
And conversely, if fatty liver is found incidentally — whether on ultrasound, CT, or MRI — it should immediately trigger a full metabolic workup, regardless of whether sugars look normal.
Key Takeaway: Elevated sugar is one of the last signs of insulin resistance. Long before sugars rise, insulin resistance has already been fueling heart disease, cancer, dementia, Parkinson’s, and fatty liver.
Why Traditional Medicine Falls Short
So why do patients so often hear, “Don’t worry, just watch your diet”? Because traditional medicine remains glucose-centric, not insulin-centric.(1,3)
But it’s more than that. Traditional medicine is disease-centric: it is programmed to treat disease after it appears and to prescribe drugs reactively, rather than identifying risk upstream, being proactive, and preventing illness in the first place.(2,6).
This mindset explains why so many people are reassured when their blood sugar is only “borderline,” instead of being warned that the fire of insulin resistance has already been smoldering for years.
During the Vietnam War, there was a famous antiwar poster that read:
“What if they gave a war and nobody came?”
I say this:
What if we actually addressed risk early — and nobody got sick?
That is the vision of functional metabolic medicine: not waiting for the house to burn, but preventing the fire altogether.
Do You Know Your Insulin Number?
We’ve all been trained to know our “numbers.” Patients can usually tell you their cholesterol. Many know their blood sugar or hemoglobin A1c. But let me ask you this: do you know your insulin number? Has anyone even tested it?
Insulin levels are often far more predictive of future disease than sugar or cholesterol, yet they are rarely checked in routine care.(3,4,8) That’s like measuring the smoke in a burning house but never looking for the fire.
This is why an oral glucose tolerance test with insulin response is so valuable — it reveals the hidden fire of insulin resistance long before sugars rise.(1,4,18).
Key Takeaway: Sugar and cholesterol numbers are common knowledge. Insulin — the most predictive number of all — is almost never measured.
The Proactive Workup Patients Deserve
At CardioCore, we believe that every patient with borderline sugars deserves a root-cause evaluation — not just a “watch and wait” approach.
Here’s the proactive roadmap:
Cardiovascular Risk First (6,18,19).
If you already have cardiovascular disease — even with normal sugars — you need a 2-hour oral glucose tolerance test (OGTT) with insulin response. (20). Studies have demonstrated that up to 88% of patients with an acute cardiovascular event and normal sugars will have an abnormal OGTT within 3 years indicating evidence of prediabetes or diabetes (20).
And if you already have a high coronary calcium score, this should automatically trigger a full metabolic workup, regardless of whether your Hemoglobin A1c looks “normal.” (21) Why? Because diabetes is considered a cardiovascular disease equivalent.(22) The fire of insulin resistance is already burning, even if sugar hasn’t risen yet.
CT Coronary Calcium Score (CAC) (6,18).
If you don’t have known heart disease, the next step is a CAC scan.
A CAC >0 means plaque is present → treat aggressively.
A CAC =0 doesn’t mean you’re “safe.” It means you still need an OGTT with insulin to detect hidden resistance.
Insulin Response Curves
A regular glucose tolerance test measures only sugar.
By adding insulin levels at fasting, 1 hour, and 2 hours, we can tell if:
You have hyperinsulinemia with normal glucose → early resistance.
You have a blunted insulin response → beta-cell failure or MODY.(4).
In fact, there is a rare subgroup of patients with an elevated A1c who do not follow the usual pattern of insulin resistance. Instead, they may have a condition called MODY (Maturity-Onset Diabetes of the Young), where the pancreas is essentially “programmed” to respond only once glucose rises to a higher set point. These patients can maintain normal insulin function but at the cost of chronically higher glucose. They generally do not show the same cardiometabolic risks seen in insulin resistance.(1).
This is exactly why the OGTT with insulin response is so important — it helps distinguish between the vast majority with insulin resistance and the very rare individuals with MODY. Those patients can then be referred for genetic testing. But keep in mind, MODY is uncommon, and for most people with borderline or high sugars, the underlying driver is insulin resistance.(1).
Liver Assessment (15–17).
If the CAC scan doesn’t clearly show the liver, a liver ultrasound should be done.
And remember: if fatty liver is found incidentally, it should always trigger a full metabolic workup.
Female-Specific Considerations (11–14).
Because insulin resistance dramatically increases cancer risk, women should:
Stay current on mammograms.
Have regular gynecologic evaluations.
Screen for uterine cancer if at risk.
Key Takeaway: Borderline sugars should never be brushed off. They should trigger a full-body workup: heart, pancreas, liver, and — for women — cancer screening.
A New Path Forward
The old model is glucose-centric: wait until sugar rises, then medicate.
The new model is insulin-centric: detect resistance early and stop the fire before it spreads.(1–4,18).
This is the philosophy of functional metabolic medicine. It goes beyond numbers on a lab report to address root causes:
Nutrition: eating patterns that lower insulin and inflammation.
Movement: strength training to build muscle, the largest sugar-burning tissue.
Stress & Sleep: reducing cortisol and restoring circadian health.
Targeted therapies: medication or supplementation chosen to address insulin resistance, not just sugar.
At CardioCore, this is not just our method — it’s our mission:
“Getting to the Core… the Path to Wellness — where being Healthy is Not an Accident.”
We don’t wait for patients to lose 90% of their beta cells before acting. We step in early, when prevention still works.
Key Takeaway: Functional metabolic medicine is proactive, root-cause care. Traditional medicine waits for sugar — the last symptom — before acting.
Conclusion: Don’t Wait for the Flames
Borderline sugars are not a mild warning. They are proof that the fire has been burning silently for years.
By the time you reach this stage:
Your pancreas has already lost ~85% of its strength.(1,4)
Elevated sugars are one of the last manifestations of insulin resistance — not the beginning.
Your risk of heart attack and stroke is already elevated.(6,18, 22).
Your cancer risk is climbing — breast cancer 20–40% higher with BMI >30, 4.6x higher with BMI >40; uterine cancer 152% higher at BMI 30–35, 345% higher at BMI 35–40, and 614% higher at BMI >40. (13,14).
Your dementia and Parkinson’s risk is rising — after genetics, high insulin is the strongest risk factor for dementia and other neurodegenerative disease.(9,10).
Your liver may already be showing fat — and MASH is now the leading cause of cirrhosis and liver transplant.
If you have a high calcium score or cardiovascular disease, you should automatically have a full metabolic workup, regardless of your A1c.(20)
And if fatty liver is found incidentally, that too should trigger a metabolic evaluation. (15–17).
The smoke (glucose) is visible. The fire (insulin resistance) has been raging for years.
At CardioCore Metabolic Wellness Center, we don’t wait for the roof to collapse. We believe in early detection, proactive intervention, and root-cause solutions.
Because being Healthy is Not an Accident. It’s a choice. It’s a path.
And that path starts by getting to the core.
Click here to book a discovery call
Click here to join our private community
Click here to speak with our CardioMetabolic virtual assistant
References
American Diabetes Association. Standards of Medical Care in Diabetes—2023. Diabetes Care. 2023;46(Suppl. 1):S1–S154.
Grundy SM, et al. Implications of recent clinical trials for the NCEP ATP III guidelines. Circulation. 2004;110(2):227–239.
Reaven GM. Insulin resistance: the link between obesity and cardiovascular disease. Med Clin North Am. 2011;95(5):875–892.
DeFronzo RA, Ferrannini E. Insulin resistance: a multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic CVD. Diabetes Care. 1991;14(3):173–194.
Emerging Risk Factors Collaboration. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364:829–841.
Grundy SM, et al. Diabetes and cardiovascular disease: a statement for healthcare professionals. Circulation. 1999;100:1134–1146.
Beckman JA, et al. Diabetes and atherosclerosis. JAMA. 2002;287(19):2570–2581.
Laakso M, Kuusisto J. Insulin resistance and hyperglycemia in CVD development. Nat Rev Endocrinol. 2014;10:293–302.
Biessels GJ, et al. Risk of dementia in diabetes mellitus: a systematic review. Lancet Neurol. 2006;5(1):64–74.
Arnold SE, et al. Brain insulin resistance in type 2 diabetes and Alzheimer disease. Nat Rev Neurol. 2018;14(3):168–181.
Giovannucci E, et al. Diabetes and cancer: a consensus report. CA Cancer J Clin. 2010;60:207–221.
Gallagher EJ, LeRoith D. Hyperinsulinaemia in cancer. Nat Rev Cancer. 2020;20:629–644.
Renehan AG, et al. BMI and incidence of cancer: a meta-analysis. Lancet. 2008;371(9612):569–578.
Calle EE, et al. Overweight, obesity, and mortality from cancer in U.S. adults. N Engl J Med. 2003;348:1625–1638.
Chalasani N, et al. The diagnosis and management of NAFLD: guidance. Hepatology. 2018;67(1):328–357.
Younossi Z, et al. Global burden of NAFLD and NASH. Nat Rev Gastroenterol Hepatol. 2018;15:11–20.
Allen AM, et al. The rising burden of NAFLD in the U.S. Hepatology. 2018;67(1):123–133.
Rydén L, et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases. Eur Heart J. 2013;34:3035–3087.
Nichols GA, et al. CVD risk in type 2 diabetes: UKPDS analysis. Diabetes Care. 2007;30(Suppl 2):S9–S13.
Jesús, M., et al. “Real incidence of diabetes mellitus in a coronary disease population.” The American Journal of Cardiology 111.3 (2013): 333-338.
Blaha, MJ. The Relationship Between Insulin Resistance and Incidence and Progression of Coronary Artery Calcification: The Multi-Ethnic Study of Atherosclerosis (MESA),Diabetes Care 2011;34(3):749–751
Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014;63(25 Pt B):2889-2934. Epub November 12, 2013. DOI: 10.1016/j.jacc.2013.11.002
