Rebuild Your Heart Health & Energy Metabolism
Where Blood Sugar, Inflammation, and Cardiovascular Wellness Meet
Don't settle for treating the tip of the iceberg - address the root causes of your cardiometabolic issues
"Getting to the Core...the Path to Wellness
- where being Healthy is not an Accident"
We look deeper than symptoms, targeting the hidden factors affecting your energy, weight, and heart health for lasting relief.
The Silent Epidemic:
Insulin Resistance
Beyond Blood Sugar
Insulin resistance exists 10-15 years before blood sugar levels become abnormal, silently damaging your body while traditional medicine waits for lab values to change.
Inflammation Connection
Chronic inflammation and insulin resistance form a dangerous partnership, creating the perfect storm for heart disease, diabetes, and cognitive decline.
Brain Health Impact
Insulin resistance is one of the strongest predictors of Alzheimer's dementia, affecting cognitive function long before symptoms appear.
Rebalancing Your Heart & Energy Systems

Nutrition
Personalized dietary strategies

Gut Microbiome Balance
Foundation of metabolic health

Genetic Expression
Your genes aren't your destiny
Transform Your Heart Health Journey Today

10-15
Years Earlier
We detect insulin resistance years before traditional tests show problems
90%
Cell Damage
By the time diabetes is diagnosed, 90% of insulin-producing cells are already damaged. The Silent Danger

2/3
Heart Disease Patients
With normal blood sugar still have insulin resistance.
Uncover hidden triggers, develop personalized strategies, and reclaim optimal health. Stop the cycle of "more drugs, worse health" and invest in sustainable wellness.
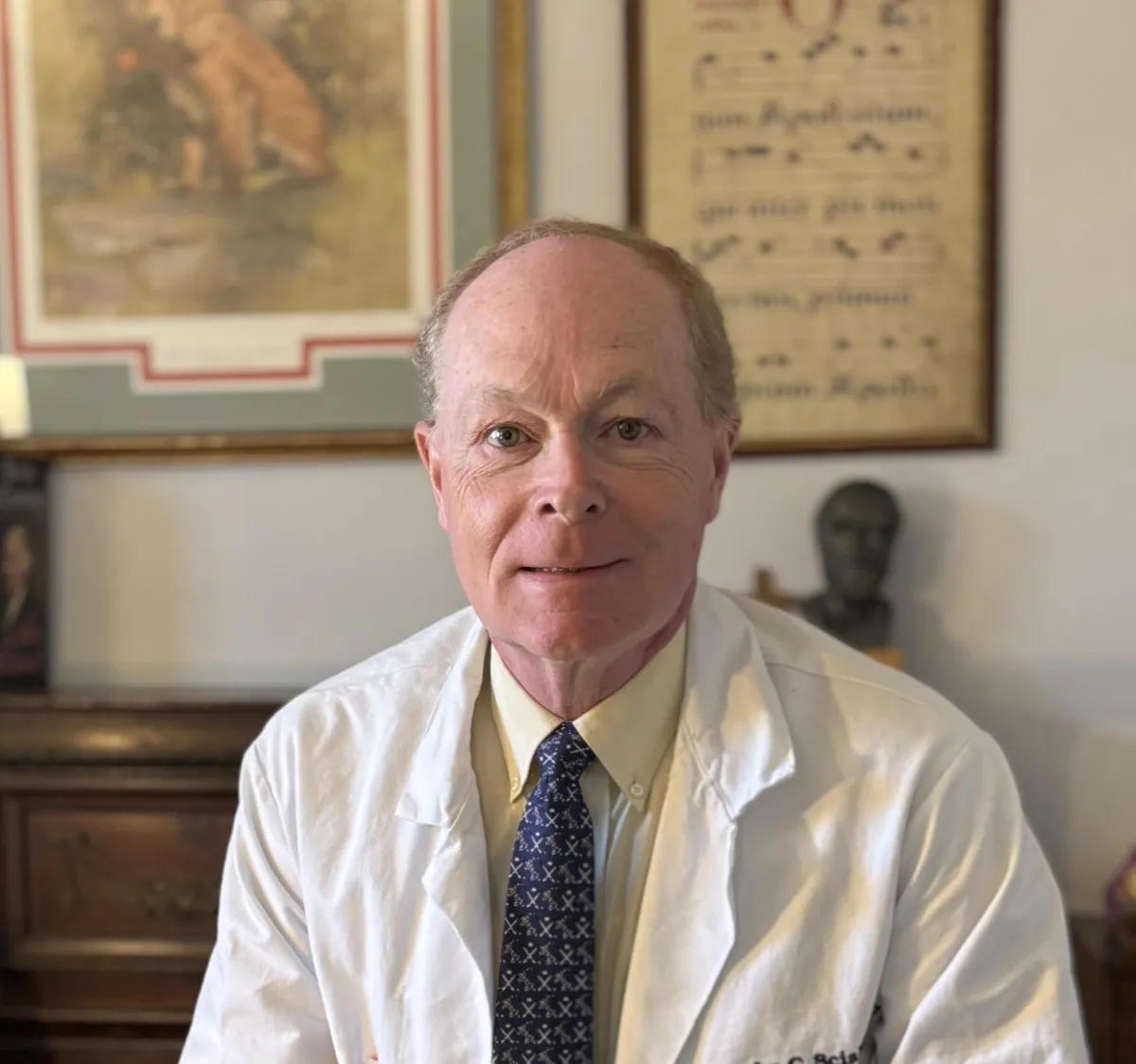
Meet John Sciales
I help restore energy and heart health when standard approaches fall short. Instead of just managing symptoms, I find what's really causing your fatigue, weight challenges, and cardiovascular concerns. By addressing these root issues, we can rebuild your body's natural balance and resilience—giving you back the vitality you deserve.
Restoring Heart & Metabolic Health
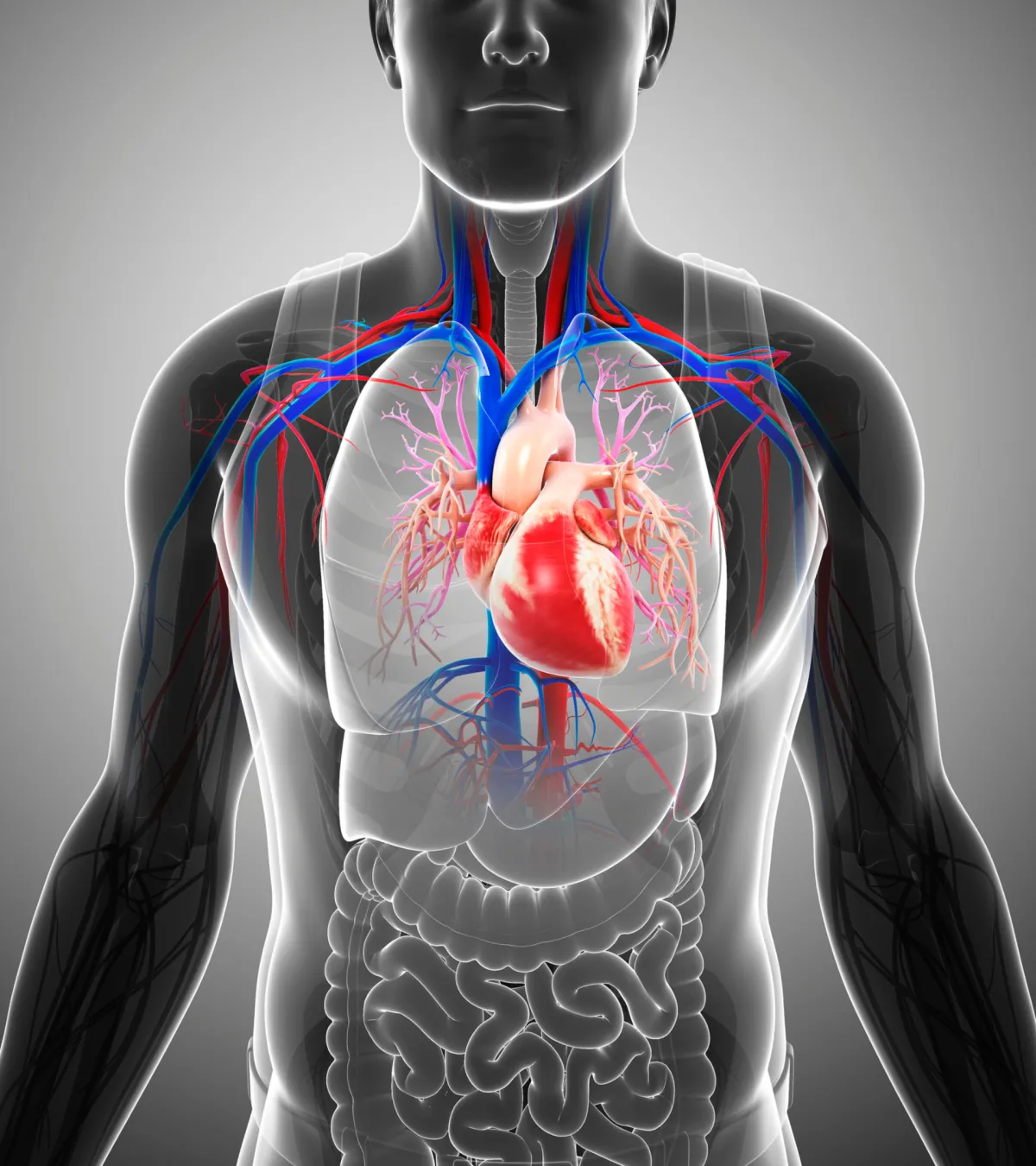
Heart Health -
Insulin resistance leads to arterial damage, hypertension, and weakened heart function
Blood Sugar Balance -
By diagnosis time, diabetes has already damaged 90% of insulin-producing cells
Metabolic Liver Function -
Insulin resistance is now the primary driver of fatty liver disease
Cardiovascular Risk -
Insulin resistance increases heart attack and stroke risk by 10-20 times
Cellular Energy Systems -
Excess insulin disrupts normal cellular metabolism throughout the body
Migraines, Metabolism & Functional Medicine: A Holistic Roadmap to Healing
Migraines aren’t random — they’re a metabolic energy crisis. Insulin resistance, mitochondrial dysfunction, and gut–brain inflammation starve neurons of fuel. Restoring metabolic health can end migrai... ...more
Functional Wellness
August 29, 2025•28 min read

How the Body Manages Fuel: Insulin Resistance, Glucose, Lactate, and the Gut Microbiome
Insulin is the body’s fuel foreman, directing energy to burn or store. When resistance develops, glucose, lactate, and gut microbes drive fatty liver, brain fog, and disease—revealing critical chances... ...more
Functional Wellness
August 28, 2025•9 min read

High Blood Pressure Unmasked: Why Metabolic Dysfunction—Not Just Your Heart—is the Real Culprit
High blood pressure isn’t just a heart issue—it’s driven by insulin resistance, inflammation, and seed oils. Lowering the cuff number isn’t enough; treating the root cause protects the heart, brain, k... ...more
Functional Wellness
August 27, 2025•6 min read
🩺 Fat, Carbs, and Heart Disease: Why Everything You’ve Been Told About Nutrition Is WRONG
New research in The Lancet dismantles the “low fat = heart healthy” myth. The real culprits are refined carbs & seed oils—not natural fats. Learn the truth about cholesterol, inflammation, and heart d... ...more
Functional Wellness
August 26, 2025•9 min read
Below the Neck, Above the Neck: How Cardiometabolic Health Shapes the Brain
What happens below the neck shapes the brain. Metabolic syndrome and insulin resistance fuel inflammation and vascular stress that raise Parkinson’s risk. The heart–brain axis is one system—waist, BP,... ...more
Functional Wellness
August 22, 2025•4 min read
Ultra-Processed Foods
Americans are eating >50% of their calories in the form of processed foods. This is a recipe for cardiometabolic disaster, fueling the chronic diseases that are plaguing Western society. ...more
Functional Wellness
August 14, 2025•8 min read
The Functional Wellness Difference
Finding Root Causes
We identify what's actually driving your fatigue, weight issues, and cardiovascular concerns instead of just treating symptoms.

Your Personal Metabolism Plan
Your body processes energy uniquely. We create a targeted strategy based on your specific metabolic patterns and heart health markers.

Science-Based Solutions
We combine proven cardiology insights with advanced metabolic testing to restore your body's natural energy and circulation systems.

Taking Control
We provide simple, practical tools to help you manage your heart health and energy levels for the long term.
Book your Complimentary Session
Schedule a free consultation with John Sciales to discuss your health goals and learn how functional wellness can help you optimize heart health, reduce stress and reclaim your energy and vitality.
Personalized Roadmap
We will create a customized plan that addresses your unique needs and helps you achieve lasting results.
Discover Our Approach
Learn if our natural approach is right for your journey.